
Dive into the world of Natural Language Processing! Explore cutting-edge NLP roles that match your skills and passions.
Explore NLP JobsCan data science be used to improve mental health? Can we use data analysis to deal with mental health problems like depression and dementia, or to monitor and improve the symptoms of impaired cognitive function, for example?
Even though data science is not being as widely used in the mental health and wellbeing sector as, say, the general healthcare, accommodation, or public services sector, we are starting to see encouraging signs indicating how it can make a very positive impact on mental health diagnosis and management.
In this expansive article, we shall discuss how data science can help us better understand the scope of the various issues faced by mental health sufferers and those working to mitigate them, some of the limitations of its use cases – and present a few case studies to show how it can impact the way mental health is assessed, treated, and managed in the not too distant future.
Mental health is a widespread problem across the globe that affects millions of people every year. The SAMHSA (Substance Abuse and Mental Health Services Administration) conducted a survey in 2019, titled Survey on Drug Use and Mental Health – where it was reported that 1 in 5 adults suffer from some form of mental illness, with women being affected more than men – 22% vs. 15%.
The NAMI (National Alliance on Mental Illness) reports that half of chronic mental illnesses may begin as early as 14.
Furthermore, the NIMH (National Institute of Mental Health) estimates that more than half of those affected by any form of mental illness do not get the appropriate treatment in time for multiple reasons – be it the accessibility or cost factor or the negative stigma usually associated with finding treatment for mental illness.
For those who do get treated, the NIMH reports that, on average, 8-10 years pass between the initial discovery of symptoms and the first treatment.
This delay in treatment can have dire effects on those suffering from mental illnesses. Unless the right treatment is administered (and on time), mental illnesses can have debilitating effects on the lives of young people, particularly teenagers. As reported by the NIMH, more than a third or 37% of teenagers who are diagnosed with a mental illness skip school as a result. The lack of life-changing opportunities that education can bring means that these young individuals often don’t have a very bright future to look forward to.
In fact, many teenagers end up making life decisions which adversely affect their future. This is why the vast majority of teens (at least 70%) who are booked into a juvenile justice system already suffer from some kind of mental illness, according to the NIMH.
This clearly shows the disturbing and often devastating effects of mental illness when left untreated – it’s something that not only affects us at the individual level but also society as a whole. Unfortunately, the increasing suicide rate among the younger population has often been linked to an existing history of mental illness – the same NIMH study also reported that 9 out of 10 young individuals who committed suicide were already suffering from mental illness.
When people suffering from mental health are unable to reach out and get the help they urgently need, they find it very hard – in fact, sometimes impossible – to get their lives back on track. The NIMH also reports that a quarter of homeless adults living in shelters already suffer from a serious mental illness or ‘SMI’, severely limiting their chances at having a normal life.
Moreover, if SMI’s are left untreated, they can have some very adverse effects on an individual’s life – for instance, the inability to work or engage in day-to-day social interactions, or being in strained relationships. This is, unfortunately, reinforced by the estimated $193.2b in lost wages as a result of SMI’s, according to the NIMH.
This correlation between suicide and mental illness is indeed a very difficult and depressing statistic, and just like the growing rate of suicide and mental illness in young people – mental illness is also causing adults to commit suicide – which is now among the leading causes of death in the US, next to heart disease, diabetes, and other health conditions.
It is indeed a sad and discouraging fact to acknowledge but mental illness around the world is not only under-diagnosed and underreported but also misunderstood. This particularly holds true for lower-income regions and developing economies around the world.
If researchers were to proactively report the number of cases pertaining to just diagnoses, countries with abundant healthcare resources and higher income levels would actually have higher incidences of mental illnesses – because the issue is becoming more and more widespread as we speak, with not enough measures in place to treat and manage it.
There is also an issue with the way these statistics are reported as ‘mental illness’ is broadly defined according to the varying definitions worldwide organisations follow when including statistics in their respective reports.
For example, a study done by the IHME (Institute of Health Metrics & Evaluation) in 2016 titled “Global Burden of Disease”, reported that 1 in 6 people around the globe suffer from at least one kind of mental illness or health condition related to substance abuse.
The WHO (World Health Organization) reported that the US has the highest occurrences of mental health disorders compared to the rest of the world. Analysis of this data revealed that 27% adults in the US suffer from some form of mental illness within a year, although this statistic was arrived upon through limited data available at the time and a variance in reporting around the globe.
Even though data science in mental health is somewhat limited at the moment, compared to other fields of medicine, it can still (at a basic level) allow researchers and data analysts to estimate the effects of mental illness with more accuracy, either according to regions and countries or on a global scale.
When these effects are understood in a quantified way and supported by real-time data, it will provide a much stronger case for the resources direly needed for mental health research, as well as for accessibility and timeliness of treatment.
Fortunately, there have been efforts to understand the value data science can bring to mental health, just like it has to other fields of medicine.
For instance, data scientists have started using ML (machine learning) to process very large data sets, hoping to find specific patterns which can help mental health service providers identify the underlying causes, signs, and symptoms of mental illnesses – so that they can choose the best possible treatment according to each unique illness.
Through the data-driven discoveries and insights, researchers can come up with the appropriate preventive measures to remedy a wide range of mental illnesses. With that said, the algorithms currently being used to accomplish such tasks need to be used more widely and constantly trained in order to perform in a consistent manner.
As data scientists and analysts continue to perfect these algorithms to achieve the above tasks, the availability of data will play a pivotal role in their success. The impact of data science on the mental health industry as a whole is a bit limited at the moment due to the current availability of data sources that are considered ‘good’, ‘reliable’, and ‘legitimate’.
Even though many organisations across the world are in the practice of collecting mental health data on a regular basis, they do so without consolidating it through a collaborative effort. We believe one of the reasons preventing this from happening is the refusal of data providers, pharmaceutical companies and health systems refusing to arrive on the same page, likely due to their varying commercial interests.
Plus, the medical professionals and scientists who are conducting extensive research into mental health illnesses are being limited by small population sizes when attempting to come up with the correct diagnosis or remedial plan – as such, they need to have access to global populations and not just a small portion of it at any given time.
Despite these setbacks and limitations, data science is actually making a very positive impact in suicide prevention, at least, which can be attributed to mental health illnesses as discussed earlier. In fact, crisis counselling emergency numbers are now using ML (machine learning), a subfield of AI, to help identify callers who may be at a high risk of harming themselves or committing suicide, according to the words they choose to communicate.
These crisis counselling hotlines and centres collect very useful information each day, such as the time of day, the day of the week, and when the most calls are received – to disperse adequate resources at any point in time to those who need them. The collected data can also help in training counsellors to understand what questions to ask callers in order to deescalate situations – and for building caller profiles who may need extra or long-term therapy which is not within the scope of the said counselling centre. Using the power of data science, counsellors can then direct callers who are at the highest risk of self-harm or suicide, to the appropriate professional so that their mental health condition can be dealt with immediately.
By combining machine learning and data analysis, data scientists can better understand the current mental illnesses that are plaguing worldwide populations, and expand their access to timely treatment and/or therapy.
The latest theories and methodologies for treatment will continue to be tested for feasibility and proven as effective or invalid – as scientists continue to collect data, but more importantly, consolidate and analyse that data properly so that the underlying algorithms can be perfected over time.
Meanwhile, major investments are being poured into initiatives, including one for better understanding the genetics that trigger mental illnesses. This neuroscience research will help medical professionals deliver better diagnosis and treatment, as well as prevent future mental health disorders more effectively.
Luckily, we are continuing to see funding into improving diagnosis which will pave the way for more effective treatments, with data science at the centre of it all to empower mental health specialists and service providers to prevent people’s mental health from getting worse, and to even prevent it from getting triggered in the first place.
Both data scientists and mental health specialists are finally coming to terms with what AI can actually do to revolutionise how mental health services are delivered. AI-powered tools are being developed to assess and diagnose a range of mental health illnesses, providing a very attractive, practical and cost-effective option for the mental health industry – as it can significantly cut down the time between diagnosis and treatment, leading to more positive results, compared to the traditional methods of diagnosis and treatment.
There’s more good news: independent studies have found that patients are now more comfortable with sharing their personal information with an AI-powered app or therapist, because it provides a certain degree of anonymity and privacy, which cannot be had when dealing with a human therapist – e.g. being judged or being talked about when not present. Some patients are very uncomfortable with this, and understandably so.
However, the effectiveness of such AI-powered tools will be (again) capped by the quality and availability of data that’s used to build the algorithms powering up the tools. Therefore, it is the responsibility of data scientists to ensure that the data sets used are reliable, diverse, and truly representative of the worldwide population of young individuals and adults who are suffering from mental illnesses.
It is imperative that mental health carers and service providers find new and practical ways of collecting data as that will be vital to the future role data science plays in mental health. Many researchers and companies alike have taken a proactive stance, experimenting with advanced AI-based tools and other technologies which can potentially improve the quality and volume of data they collect on a day-to-day basis.
This technology will help them collect data while patients are going about their normal routines, which researchers are saying will effectively eliminate recall bias. However, it is important for the developers of such technologies to work closely with both mental health professionals and researchers to establish the importance of different data types – e.g. what kind of data is most useful in diagnosing, remedying, and preventing all kinds of mental illnesses.
The current technological advancements will greatly influence the role of data science in mental health research. Verily, a company focusing on the development of technology to collect health data, recently had its team of researchers reach out to mental health professionals to openly support the application of data science in the diagnosis, treatment, and prevention of mental illnesses. This is an important step in the right direction, because it would mean that those working in the mental health field will rely less on subjective observations and much more on evidence-based research by tapping into the power of data science.
The main advantage of doing that, of course, would be far less variability in mental health diagnoses and treatments as that is a persistent issue at the moment.
The latest technology in wearable monitoring devices, for example, will allow mental health practitioners and service providers to gather huge volumes of data outside their clinical confines – by measuring and tracking daily patient activity, behaviours, and other mental health metrics throughout the day. Such technological developments will definitely improve the variety and volume of data available, ultimately, enabling researchers to tap into the power of data science to test and identify learnings in the most reliable way possible, in order to holistically benefit the field of mental healthcare and wellbeing.
Using EHR and responses from a depression questionnaire, researchers at the Mental Health Research Network built an analytics model which can predict the risk of suicide within 90 days of a mental health clinical visit.
The model enabled researchers to identify patients who were at the highest risk through specific predictors such as substance use, past suicide attempts, emergency room care, and scores on the questionnaire.
EHRs can allow data scientists to developer very accurate models, with the Kaiser Permanente researchers from the Mental Health Research Network using their model to identify 5% of the population who were at a highest risk of suicide.
Within the 5%, 43% were at high risk who had made previous suicide attempts while 48% had died from suicide. This is a notable improvement from previous models that merely predicted 1^1/2^ to 1/3 of attempted suicides vs. suicide deaths. The study illustrates how data science can help to identify the risk of death in high risk patients – although the long-term goal is to use this approach to incorporate analytics which will help develop specific treatment plans and follow-ups for those who are at a higher risk and require long-term treatment.
Crisis Text Line (CTL) is a well-known non-profit crisis counselling centre based in New York, responding quickly to text messages sent by those suffering from a mental health disorder or contemplating suicide.
Since its inception in 2013, the non-profit has exchanged around 30 million text messages with users from all over the US, adding to the wealth of data they have on mental health patients. At present, this data is being collected and organised for the early detection of self-harm and/or suicidal tendencies not catered to by the CTL facility.
Through the analysis and collection of this data, data scientists have discovered specific patterns in the language used by patients when communicating with counsellors – sharing the patterns with the general public so that a much larger segment of the population can be treated when they suffer a mental health crisis.
CTL collects three kinds of data: the actual text-based conversations patients have with the counsellor, and following the interaction, feedback from both the person who texted as well as the counsellor. Data scientists analysed this data to identify some very valuable patterns. For instance, they were able to pick up keywords like “Ibuprofen” or “Advil”, which indicated a high risk of suicide as opposed to other words only which were attributed to suicide, such as “kill”, “die”, or “cut”.
This clearly illustrates how ML technology can be far more effective than the human intuition used by mental health providers to detect the risk of deteriorating mental health and suicide.
The University of Southern California’s Institute of Creative Technologies has come up with a 3D chatbot, Ellie, to fulfil the role of a virtual therapist capable of showing facial expressions and detecting non-verbal cues from patients through algorithms. The data fed into Ellie through patients' verbal input and facial expressions helps her determine the ideal visual and verbal response through these algorithms.
Military personal returning from duty in Afghanistan were tested for PTSD (Post Traumatic Stress Disorder) symptoms – where Ellie proved to be more effective compared to the military’s standard health assessment routine.
Researchers observed how the soldiers' ability to trust Ellie and build rapport with her was pivotal to success. Over 60% of US counties don’t have a psychiatrist within their borders while 40% of the US population resides in areas with an acute shortage of mental health professionals.
Ellie is one example of how data science in mental health can be accessible to all, in order to positively impact the mental health of those who require timely intervention and treatment, and even prevent mental health issues from triggering.
Interested in learning more about the implications of data science in mental health? Our data scientists are always available to consult and discuss the ways in which the quality of mental healthcare services can be improved: +44 20 3488 5740.
Tags
Data science mental health
Meta description: Data science and mental health: Saving lives and wellbeing
Breakthroughs in data science for mental health and wellbeing management can help to save lives and pave the way for a healthier, more productive societies.
Looking for experts in Natural Language Processing? Post your job openings with us and find your ideal candidate today!
Post a Job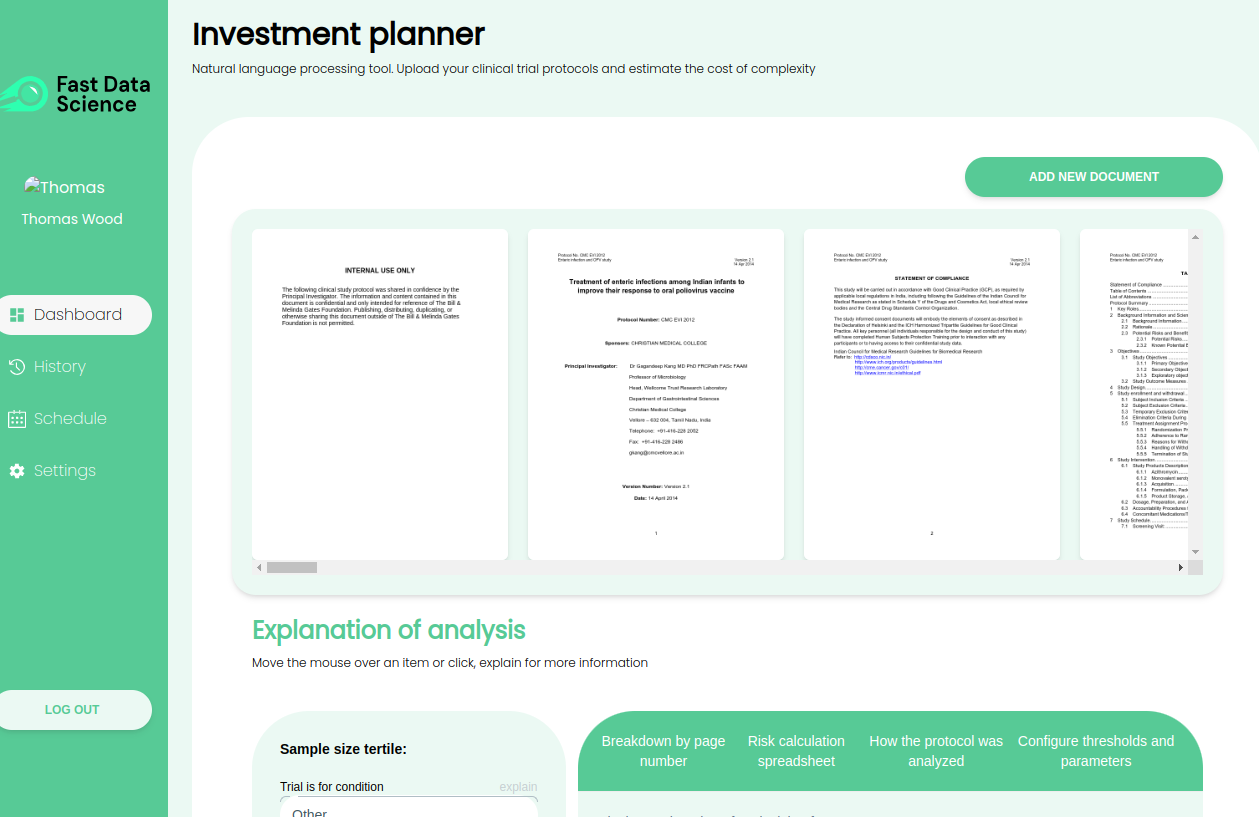
Modelling risk and cost in clinical trials with NLP Fast Data Science’s Clinical Trial Risk Tool Clinical trials are a vital part of bringing new drugs to market, but planning and running them can be a complex and expensive process.
What we can do for you